At first glance, the results sound paradoxical: in patients with a certain form of heart failure, the molecular motors of the heart muscle cells, the so-called myosin complexes, are often chemically altered at certain areas and can thus perform better. Researchers at Heidelberg University Hospital (UKHD) and the Herz- und Diabeteszentrum Nordrhein-Westfalen (HDZ NRW), Bad Oeynhausen (Ruhr University Bochum) have found this out and also discovered which enzyme is responsible for this. The working group led by the Heidelberg cardiologist Professor Benjamin Meder assumes that the newly described regulatory mechanism should counteract the fatigue of the heart muscle. It could thus open up a new starting point for the treatment of heart failure. The results have been published online in the journal Nature Communications and were awarded by the German Centre for Cardiovascular Research (DZHK).
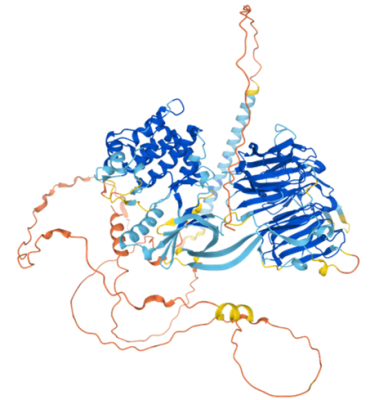
As molecular motors, myosins ensure that the heart muscle cells contract evenly. By changing their shape, they move certain elements of the cytoskeleton, the actin filaments, against each other: the heart muscle cell contracts. Chemical modifications of these proteins are an important regulatory mechanism for the heart muscle cells to be able to react to changed stresses. So-called phosphorylations, the attachment of additional phosphate groups to the protein, have a positive effect on the contraction force of the cells and provide a force boost during stronger stress.
Modifications discovered in certain forms of cardiac insufficiency
The research group led by Professor Meder and Dr Marion Müller developed a special measurement method to detect phosphorylations of a small protein of the contractile apparatus, the essential myosin light chain (ELC). "We were surprised to find an increased proportion of protein phosphorylations on the essential myosin light chain in patients with so-called dilated cardiomyopathy, of all things," says first author Dr Müller, who has since moved from the UKHD to the Agnes Wittenborg Institut für translationale Herz-Kreislaufforschung at the HDZ NRW. Dilated cardiomyopathy is a chronic heart disease in which the heart muscle virtually swells and continuously loses pumping power. Dr Müller suspects: "The modifications could be an attempt by the heart cells to compensate for the increasing loss of function." The team identified a total of nine phosphorylation sites on the comparatively tiny ELC protein.
The scientists also identified the originator of the modifications and thus an important player in this regulatory mechanism: the enzyme "NIMA-associated kinase 9" (NEK9) is found in a high proportion in the left heart muscle of humans, binds to the ELC protein and regulates phosphorylation. Experiments on zebrafish confirmed the key role of NEK9: in genetically modified animals lacking a certain part of the enzyme, phosphorylation and thus the adaptation of heart function failed, they developed cardiac insufficiency. "This regulatory mechanism literally electrochemically charges the heart motors and could potentially be used for drug therapy in heart failure by supporting heart function via an increase in ELC phosphorylation," says principal investigator Meder, Professor of Precision Medicine at the Department of Cardiology, Angiology and Pneumology at the UKHD.
The research work was carried out at the UKHD as part of a project funded by the German Research Foundation and the German Centre for Cardiovascular Research (DZHK) and in close collaboration with the HDZ NRW, Bad Oeynhausen. Further collaboration partners are the "Core Facility for Mass Spectrometry & Proteomics" of the Centre for Molecular Biology at the University of Heidelberg, the Clinic and Polyclinic for Cardiology at the Leipzig University Hospital, and the "Genome Technology Center" of Stanford University, USA.
Original publication:
Müller, M., Eghbalian, R., Boeckel, JN. et al. NIMA-related kinase 9 regulates the phosphorylation of the essential myosin light chain in the heart. Nat Commun 13, 6209 (2022). https://doi.org/10.1038/s41467-022-33658-2
Source: Press release Heidelberg University Hospital