Over time, high blood pressure leads to kidney damage – unless you happen to have a mutated PDE3A gene. “This mutation causes extremely high blood pressure, but the kidneys still work normally even after years of having the condition,” says Dr. Enno Klußmann, head of the Anchored Signalling Lab in Berlin. He and his team at the Max Delbrück Center and at the German Center for Cardiovascular Research (DZHK), have now published their results in “Kidney International.”
Getting to the heart of the matter
Last year, the researchers discovered that the gene mutation responsible for causing extremely high blood pressure and short fingers (hypertension and brachydactyly, or HTNB) also protects the heart from hypertension-induced damage. Only the brain remains vulnerable: “Without treatment, patients with HTNB – a genetic disease that occurs in just 10 to 20 families globally – tend to die relatively young from a stroke,” says Klußmann. “So even children have to take antihypertensive drugs to control their blood pressure.” But with medication, it can still be hard to bring the blood pressure down to a normal level.
After discovering that the mutated PDE3A gene protected the heart, Klußmann and his team began investigating the kidneys of a female patient in Germany and of two HTNB rat models. The patient is receiving treatment from Dr. Stephan Walter at MVZ Nierenzentrum Limburg, a specialist kidney center. The rat models have the same PDE3A mutation as human patients (PDE3A stands for the enzyme phosphodiesterase 3A) and were developed by researchers led by Professor Michael Bader. Bader heads the Molecular Biology of Peptide Hormones Lab at the Max Delbrück Center. He and Walter are also authors of the latest study.
All parameters in the normal range
In patients with severe HTNB, the PDE3A gene is mutated in two places and these mutations cause the encoded enzyme to become hyperactive. “We don’t yet fully understand why that happens, or how the mutation damages the vessels and the brain while protecting the heart and the kidneys,” says Klußmann.
He and his team could, however, show that the kidneys of the Limburg patient are working perfectly normally. “We found that the secretion of renin – a hormone-like enzyme that’s produced in the kidneys and heavily involved in controlling blood pressure – is actually suppressed in her case,” says Anastasiia Sholokh, a researcher in Klußmann’s team and lead author of the study. “Her aldosterone levels are normal.” Aldosterone is a hormone made in the adrenal glands. Like renin, it can cause blood pressure to rise. “Conventional parameters of kidney function like glomerular filtration rate and albumin levels in the blood and urine also indicate that her kidneys are healthy,” says Sholokh.
Imitating the mutation’s effects
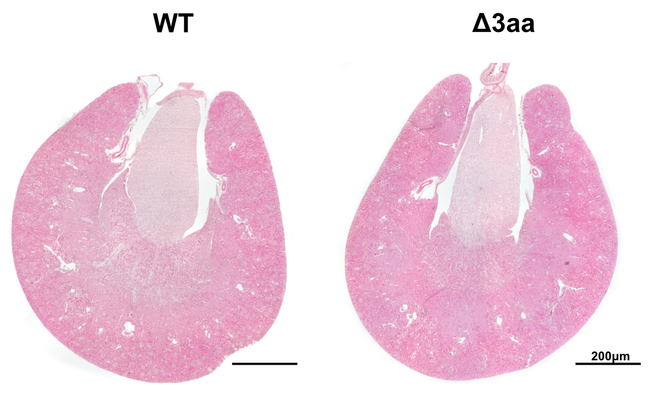
The kidney tissue in the HTNB rats also showed no signs of inflammation or fibrosis (an increased production of connective tissue that causes organs to harden). The transcriptome, which shows what genes are currently active, was also unchanged in the rats’ kidneys. “What we did find is reduced expression of the protein amphiregulin in certain regions of the organ,” says Sholokh. “Since high levels of amphiregulin are likely to damage the kidneys, the suppressed production probably helps to protect them.”
“We showed that hypertension doesn’t always automatically lead to kidney damage,” says Klußmann, summing up. “Now we want to examine the protective effect of the mutated PDE3A gene and see if we can mimic it with appropriate therapeutic agents.” This could eventually help patients with hypertension avoid developing chronic kidney disease.
Publication: Anastasiia Sholokh et al. (2023): „Mutant PDE3A protects the kidney from hypertension-induced damage“. Kidney International, DOI: 10.1016/j.kint.2023.04.026
Scientific contact: Enno Klußmann, Leiter der Arbeitsgruppe „Ankerproteine und Signaltransduktion“, Max-Delbrück-Centrum für Molekulare Medizin in der Helmholtz-Gemeinschaft (MDC), enno.klussmann(at)mdc-berlin.de
Source: Press release Max-Delbrück-Centrum für Molekulare Medizin in der Helmholtz-Gemeinschaft (MDC)