The so-called "cloaked" cells can hide from the immune system. Prof. Thomas Eschenhagen from the University Medical Center Hamburg-Eppendorf explains why this is important: “If you apply cardiac tissue that is foreign to the body, it will be recognized and rejected if you are not given immunosuppressive drugs at the same time. The cells available to Evotec have modified certain immune factors so that the recipient's immune system can no longer reject them. This means that the cells fly under the radar, so to speak, immunosuppressants would then not be necessary or only in a lower dose. "
Such methods have been developed in recent years by various research groups, including Sonja Schrepfer's group from the UKE and the University of San Francisco (Nature Biotechnology 2018). In the meantime, the various approaches are being further developed by companies, and Evotec has secured the license for cells from panCELLa.
Cell therapy with heart tissue from stem cells
Eschenhagen and his team have been researching for over twenty years to heal sick hearts with new heart tissue. Because once myocardial cells are destroyed, they never grow back. Heart muscle weakness occurs, which means that the heart's pumping power and thus the patient's performance are - sometimes extremely - limited. The most common reason for heart failure is a previous heart attack. The weak heart cannot be cured.
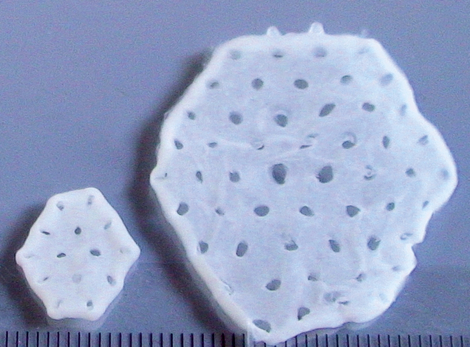
After years of basic research, the Hamburg team's cell therapy is now on the way to clinical application. And this is how the tissue is made: So-called induced pluripotent stem cells (iPSC) - these are cells from which researchers can create any body cell - are turned into living heart muscle cells in the laboratory. The palm-sized heart muscle tissue is grown from this and sewn onto the diseased heart.
Cells have safety mechanisms
And the DZHK researchers want to try out another ingenious principle: the stem cells used by Evotec are modified in such a way that they can be specifically killed with a drug that is approved and frequently used for human use if they are in the state of cell division. Basically, the heart cells are produced from the iPS cells in a highly controlled process in such a way that there are no more cells in the implanted product that are not fully differentiated, i.e. can still divide. Because such cells could possibly lead to the formation of a benign tumor. As an additional safety option, the stem cells are now genetically modified in such a way that any dividing cells that may still be present are specifically eliminated by the drug. The implant is not affected because heart muscle cells do not divide.
"We need industrial partners to manufacture heart muscle tissue for people, university laboratories are not equipped for this," says Eschenhagen. Evotec has built an industrialized iPSC infrastructure that is one of the largest and most modern of its kind in the industry. The listed company with headquarters in Hamburg has been working flat out on regenerative therapy projects for several years. The preparatory work leading to the cooperation with Evotec was financed to a large extent by the DZHK.
Eschenhagen is not afraid of contact with such partnerships with industry, on the contrary: “Only companies can produce pharmaceutical quality material on a larger scale. For the successful translation, i.e. the transfer of academic research results into clinical application, such cooperation is essential. "Transparency is the top priority, says Eschenhagen. He personally has no shares in Evotec.
Original Publication: Human Engineered Heart Tissue Patches Remuscularize the Injured Heart in a Dose-Dependent Manner. Weinberger et al. Circulation 2021
Scientific Contact: Prof. Thomas Eschenhagen, Universitätsklinikum Hamburg-Eppendorf, t.eschenhagen(at)uke.de
Contact: Christine Vollgraf, Leiterin DZHK-Pressestelle, Tel: 030 3465 52902, christine.vollgraf(at)dzhk.de
Translational Research Project: IPSC-EHT transplantation for cardiac repair – towards first-in-patient

![[Translate to English:] Menschliches Herz](/fileadmin/_processed_/0/c/csm_AdobeStock_6165264_003da97b56.jpg)